How Medically Integrated Dispensing Improves Access, Care Coordination and Patient Outcomes

As a pharmacist, I have always been inspired by the idea of specialty pharmacy and how it approaches patient care. Now at House Rx, I have the opportunity to improve this care delivery model through medically integrated dispensing (MID) and improve patient access to life-changing medicines.
At its core, specialty pharmacy was conceived to take better care of patients – to provide those who are most vulnerable, especially those with chronic and complex medical conditions – with a support system to help them navigate a convoluted healthcare system.
But let’s face it. A wide gulf exists between the promise of speciality pharmacy and how it really works. The truth is specialty pharmacy today doesn’t work flawlessly or seamlessly for the patient. Too often the patient AND the care team report they are dissatisfied with the experience. Patients are often delayed in initiating therapy and are overwhelmed by the financial toxicity of specialty medications, while care teams are overburdened by the administrative hassle of getting patients on therapy and lack the visibility to control their patients’ adherence. This illustrates that the model isn’t succeeding at its overall goal of providing high-touch, patient-centric care. It reveals that the pharmacist doesn’t always have the tools to do their job effectively and may be operating siloed from the care team, inhibiting the ability to collaborate, ask questions and provide answers.
This problem is becoming increasingly more acute as the number of patients requiring treatment with specialty medication grows. Specialty pharmacy care has to be re-imagined to truly be different as a care model, realize its full impact on patients and make good on the bet that higher touch pharmacy care will yield better results. Enter medically-integrated dispensing.
MID and the Role of the Pharmacist
The MID care model is designed around the patient to improve access to care and better clinical outcomes. What I love most about MID is that it recognizes the role of pharmacists as a critical member of the care team. By having pharmacists play a more hands-on, active role in the patient’s care journey — and work in lockstep with the patient’s medical team — the bet is that patients will do better. This is a very inspirational calling for pharmacists, and it motivates me every day to improve and enhance our role as a provider of patient care.
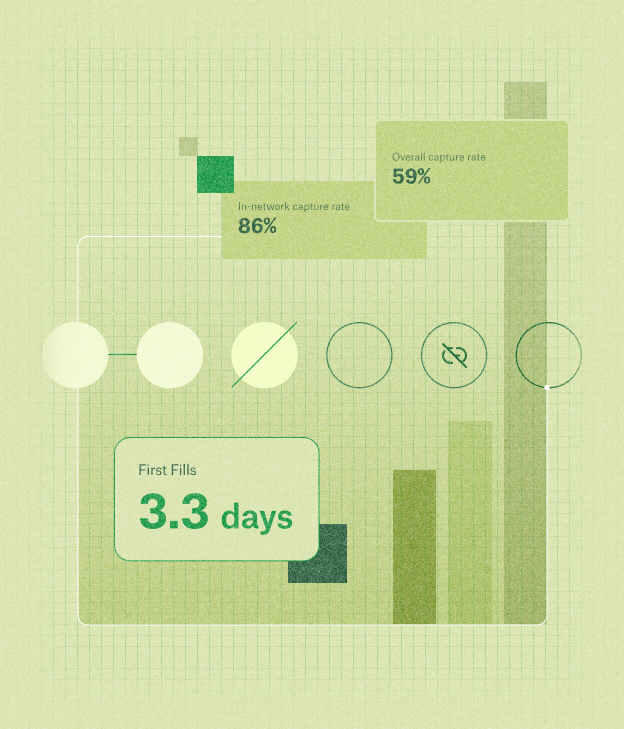
Conceptually, the MID care model is simple. The workflows involved in this care model focus on getting patients access to their medication more efficiently by helping them navigate the complex prior authorization and financial assistance processes required to obtain these often life-saving (and extremely expensive) therapies. In a traditional specialty pharmacy model, getting a patient their medication — and further getting the patient to adhere to their medication — is the responsibility (and too often the burden) of the patient. MID flips the responsibility to the care team. By including pharmacists as part of this team, the model enables the pharmacist to actively support the care team by ensuring that the treatment is appropriate and that the patient is empowered with education to take the medication appropriately.
But the MID model goes beyond just getting patients on their medication efficiently. Throughout the course of treatment, the pharmacist participates in patient monitoring to confirm that the therapy remains appropriate and effective. While it may seem subtle, this is an important shift in responsibility which historically has been placed on the prescriber & medical team. In MID, this important practice becomes a collaboration between the prescriber and the pharmacist.
The Role of Technology
For this model of care to be successful, an important part of the equation is rethinking how we leverage technology to share critical clinical information between these team members so everyone has the most up to date picture of the patient’s health. This was the challenge that drew me to House Rx.
With the right technology, pharmacists are better equipped to thoroughly and accurately assess, monitor, and educate patients throughout the course of treatment. Similarly, physicians are better informed with the often elusive knowledge of exactly when their patients receive medication and how they are doing on treatment between visits. The relationship between provider and pharmacist becomes less transactional and more collaborative, resulting in better patient care.
Utilizing technology to break down silos that exist and facilitate collaboration between physicians, pharmacy, and patients ultimately enhances every step of the MID workflow, in turn helping patients clear all the hurdles between when their provider prescribes therapy and when they can initiate that therapy. This is the type of technology stack that we have set out to build at House Rx through a collaboration between pharmacists, physicians, engineering and product experts.
It’s simple: Patients are better off when the people taking care of them work together. Medically-integrated dispensing can restore the promise of specialty pharmacy by bringing the full care team together under one proverbial roof.







.jpg)